Subscribe to the monthly blog
Join our community and get regular emails on Gut Health, Stress Management, Nutritional Strategies and Health Habits.
Library
Leaky Gut Syndrome
Most people think of their gut as just a digestion machine. But it’s far more than that—it’s the command centre of your immune system. When the gut lining is compromised, it can trigger a silent war beneath the surface. A war that can lead to bloating, fatigue, food intolerances, and in more serious cases, autoimmune-like gut disorders.
Let’s unpack how this breakdown happens and how you can start restoring your gut’s integrity with targeted, natural strategies.
Your Gut Wall: A Smart Security System
Imagine your gut lining like a high-tech security fence. It’s made of a single layer of tightly packed epithelial cells, reinforced by a mucosal lining—a slick, gel-like layer that acts as a buffer zone between the outside world (your food and microbes) and your inner world (your immune system).
This fence is designed to be selectively permeable, letting nutrients through while blocking pathogens, toxins, and undigested proteins. But when this barrier breaks down due to chronic stress, poor diet, alcohol, medications, or infections, the fence becomes porous.
Now, invaders start slipping through the cracks.
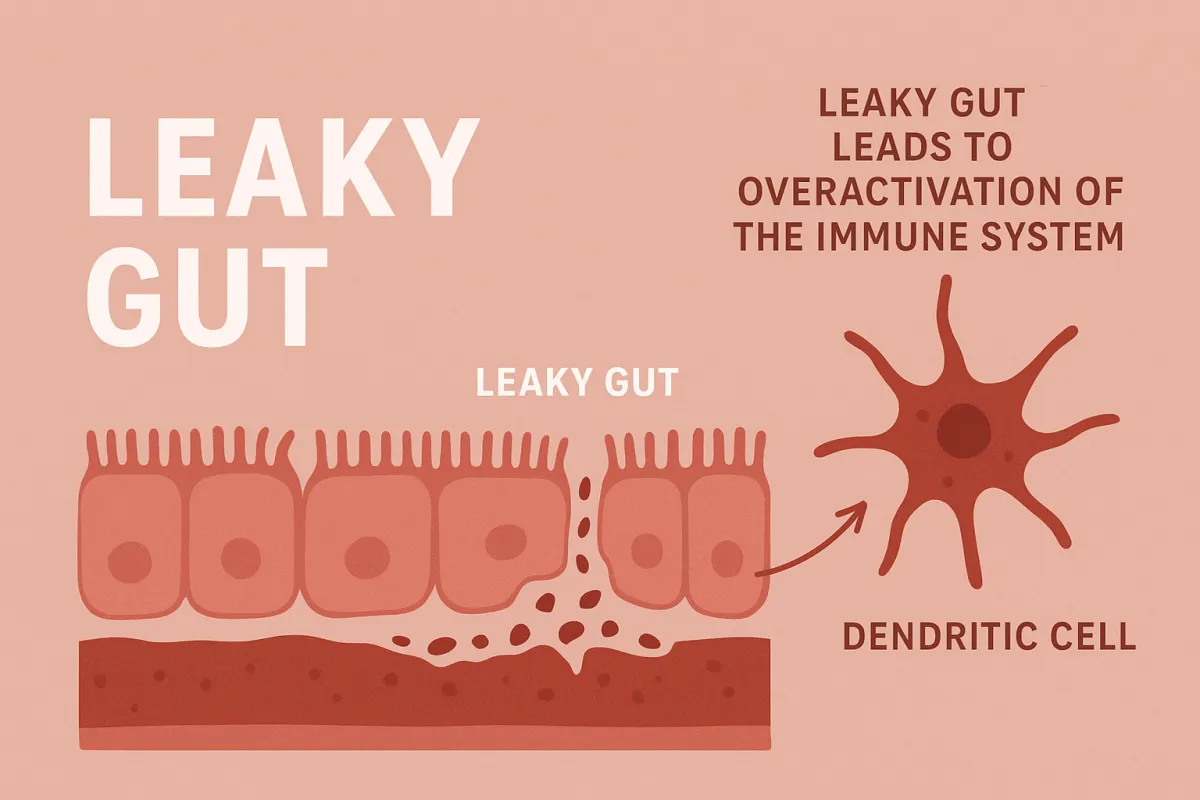
Dendritic Cells: The Gut’s Surveillance Team
Lurking just beneath the gut lining are your immune system’s scouts, dendritic cells. They’re like border patrol agents, constantly sampling what’s happening on the other side of the wall.
In a healthy gut, the mucosal lining buffers these cells from direct contact with everything passing through your intestines. But when the mucosal barrier thins, dendritic cells stretch their “arms” through the gut wall and come into direct contact with food particles, bacteria, and toxins.
This is where the system backfires. These scouts raise the alarm, even when there’s no true threat—triggering a cascade of immune responses.
Macrophages and the Inflammation Cascade
When dendritic cells sound the alarm, they call in reinforcements, macrophages. These are your immune system’s cleanup crew, designed to engulf and destroy invaders. But under constant activation, they go from helpful to harmful.
Think of it like a smoke detector that won’t stop blaring. The macrophages flood the area with pro-inflammatory cytokines, damaging the gut lining even further. This inflammation increases permeability, which creates more immune activation, a vicious loop.
Over time, this can manifest as:
Chronic bloating and gas
Food sensitivities
Brain fog and fatigue
Diagnosed autoimmune-like GI disorders (e.g. Crohn’s, colitis)
This isn't just irritation—it's immune dysregulation driven by barrier breakdown.
Repairing the Barrier: Natural Strategies That Work
The good news? The gut has an incredible ability to repair itself—if given the right inputs. Let’s look at how to stop the fire and start the rebuild.
🔹 1. Green Tea (EGCG)
One of the most researched herbal compounds, epigallocatechin gallate (EGCG) from green tea:
Supports intestinal cell regeneration
Modulates immune response by calming dendritic cells and T-cell overactivation
Reduces inflammatory cytokine production
Dosage: 250–400 mg EGCG per day (or 2–3 cups of strong brewed green tea)
🔹 2. Slippery Elm & Marshmallow Root
These demulcent herbs act like a protective balm across the gut lining. They:
Soothe inflamed mucosa
Increase mucus production to reestablish the buffer
Reduce direct antigen contact with epithelial cells
Best taken as powders or teas, especially before meals
🔹 3. L-Glutamine
This amino acid is the preferred fuel source for enterocytes (the cells that make up your gut lining). It:
Supports tissue repair
Helps tighten loose junctions
Enhances mucosal immunity
Dosage: 5–10g per day, best taken away from meals
🔹 4. Curcumin
The active compound in turmeric, curcumin:
Downregulates NF-kB (a key inflammatory switch)
Reduces macrophage activation
Promotes gut microbial diversity
Use highly bioavailable forms like curcumin phytosome or with piperine
🔹 5. Zinc Carnosine & Quercetin
These lesser-known compounds help reinforce the physical barrier:
Zinc carnosine promotes mucosal healing and tight junction strength
Quercetin stabilises mast cells and modulates immune activation
The Rebuild Roadmap
To truly repair and restore your gut, follow this three-phase process:
Remove – Cut out known irritants (alcohol, processed foods, NSAIDs), and consider food sensitivity testing if symptoms persist.
Repair – Implement the herbal and nutraceutical strategies outlined above consistently for 4–12 weeks.
Rebalance – Support your microbiome with fermented foods, fibre, and potentially probiotics once inflammation is controlled.
Final Thoughts: From Inflammation to Resilience
You don’t need to live in fear of your food or your immune system. But you do need to respect the complexity of the gut-immune connection.
When the barrier breaks, the immune system stops recognising friend from foe. The key to healing isn’t suppression—it’s restoration. Through strategic support, you can rebuild the fence, calm the immune response, and return your gut to a state of tolerance and strength.
Fix the lining, calm the fire, and rebuild your foundation of health.